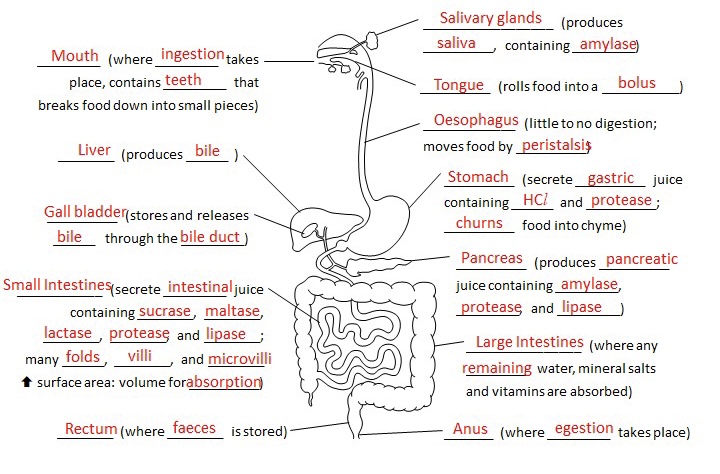
- consists alimentary canal (hole) and organs associated with it
Stages of Nutrition
- Ingestion -> mouth
- Digestion -> mouth, stomach, small intestines
- Absorption -> Small & Large intestines
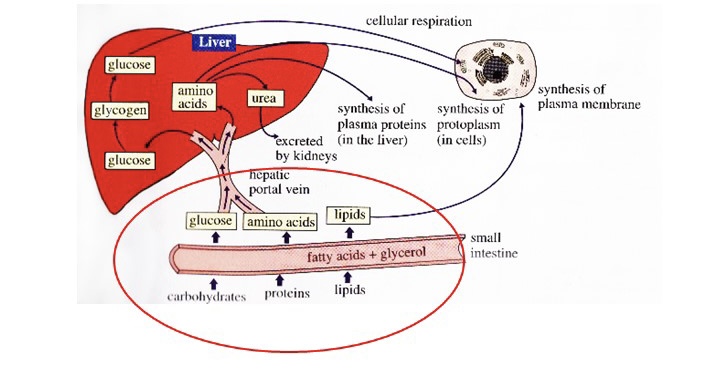
- Assimilation -> liver, body cells
- Egestion -> Rectum, Anus
- Ejection of undigested matter
| Egestion | Excretion |
|---|---|
| Not metabolic waste | Metabolic waste |
| e.g. feces | e.g. carbon dioxide, urine |
Ingestion
- Food enters body through the. mouth, which leads into the buccal cavity (mouth area)
- Digestion of food begins in the mouth by the teeth, salivary glands and tongue
Buccal cavity
- Chewing action of teeth breaks up larger pieces of food into smaller pieces
- The tongue rolls the food into small, slippery, round masses or boli
- Saliva softens food and contains salivary amylase that digests starch to maltose
- The salivary glands in the mouth secrete saliva, pH 7, which is mixed by the tongue
Physical Digestion
- Teeth
- Chewing breaks down food into smaller pieces
- increase surface area to volume ratio for chemical digestion
- Tongue
- Mixes food with saliva and rolls food into small round masses called bolus
- Saliva
- Moistens food for easier swallowing and rolling
Swallowing*
- The food bolus passes from the mouth to the pharynx and into the oesophagus
- Flap called epiglottis covers the windpipe, preventing the food from entering it
Oesophagus
- muscular tube
- channels food to the stomach
- Walls are made of 2 layers:
- Longitudinal (outer) muscles
- Circular (inner) muscles
- Muscles fibres are circular
- In ring shape
- Food moves down the oesophagus via peristalsis
- Very little chemical digestion takes place
- Peristalsis aids in physical digestion of food
Peristalsis
- rhythmic, wave-like muscular contractions
- in the wall of the alimentary canal
- longitudinal muscles and circular muscles are antagonistic
- When one contracts, the other will relax.
- e.g. biceps and triceps
| Circular muscles | Longitudinal muscles | |
|---|---|---|
| Benind the bolus | Contract (Tube narrows) | Relax (Tube lengthens) |
| In front of the bolus | Relax (Tube widens) | Contract (Tube shortens) |
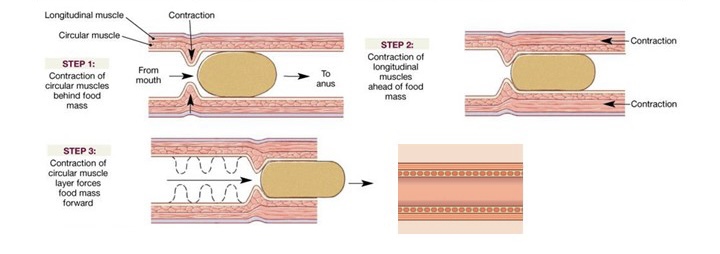
- helps food move along the gut
- Enables food to be mixed with digestive juices
Stomach
- muscular organ lined with folds and ridges on the internal surface
- Entrance and exit controlled by two sphincter muscles
- 2 pH cuz
- Physical digestion:
- Churning action in stomach
- Chemical digestion:
- Gastric juice excreted by
- Contains HCL, mucus and the protease
- HCL optimum pH for action of protease and kills harmful microorganisms in food
- protease in gastric juice catalyse the break down of proteins into polypeptides
- takes 2-3 h to convert bolus to chyme
- Why not digest itself
- Mucus lining secrete alkaline bicarbonate, that neutralises the acid pH
Stomach ulcers
- meals not eaten regularly
- gastric juice will digest stomach lining if not mixed with food
- Gastric meds contain bases and carbonates
Stomach surgeries
- Adjustable gastric band procedure
- Roux-en-Y Gastric Bypass
- Reduce fat digestion
Small Intestine
- Food passes from stomach to small intestine
- consists of the duodenum, jejunum and ileum
- 7m long in an adult
- Bulk of chemical digestion occurs in first part
Associated organs
- Liver:
- produces bile liquid
- Gall bladder:
- stores bile before releasing
- bile released from bile duct
- Pancreas:
- secretes pancreatic juice
- produce lipase
Action of Bile
- bile salts breaks up large fat globules into small fat droplets
- increases SA:V ratio
- emulsification
- NOT A CATALYST!!! ONLY INCREASES SA:V RATIO!!!!
- Cuz no chemical change
- Only physical digestion
Digestion in Small Intestine
- intestinal juice, pancreatic juice and bile secreted into the small intestine
- all alkaline, helps neutralise the acidic chyme
- pancreatic juice contains pancreatic amylase, pancreatic lipase and pancreatic protease (tripsin)
- works on larger molecules
- intestinal juice secretes:
- maltase
- sucrase
- lactase
- intestinal protease
- intestinal lipase
- works on smaller molecules Carbohydrate digestion:
| Source | Enzyme | Mode of action |
|---|---|---|
| Pancreas | Amylase | Starch -> Maltose |
| Glands on epithelial lining of small intestine | Sucrase | Sucrose -> Glucose + Fructose |
| Glands on epithelial lining of small intestine | Maltase | Maltose -> Glucose |
| Glands on epithelial lining of small intestine | Lactase | Lactose -> Glucose + Galactose |
Protein digestion:
| Source | Enzyme | Mode of action |
|---|---|---|
| Pancreas | Protease | Protein -> Polypeptide |
| Intestinal | Protease | Polypeptide -> Amino Acids |
Fat digestion:
| Source | Enzyme | Mode of action |
|---|---|---|
| Pancreas | Lipase | Glycerol + 3 Fatty Acid Chains |
| Intestinal | Lipase | Glycerol + 3 Fatty Acid Chains |
Absorption
- Long channel increase time for absorption
- folds, villi and microvilli increase SA:V, highly branched
- Villi:
- One cell layer of microvilli to separate from blood
- short diffusion distance
- Adaptations:
- Digested food substances transported away from the blood capillaries and lacteals to maintain concentration gradient for diffusion
- Glucose and amino acids absorbed into blood capillaries by diffusion or active transport
- Water, mineral salts & vitamins are also absorbed
- SMALL INTESTINE RESPONSIBLE FOR MOST WATER ABSORPTION
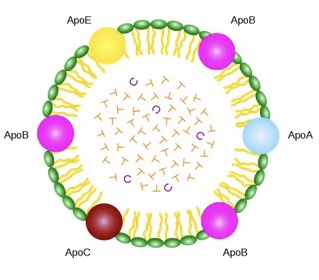
- Fats:
- glycerol and fatty acids diffuse into epithelial cells
- recombine to form fats
- packaged into special lipoprotein structure
Assimilation
- conversion of absorbed food substances for growth, reproduction and repair
Large Intestine
- consists of the colon and the rectum
- about 1.5m long
- appendix is useless
- Undigested food moves along the gut, solidifies and turns into faeces
- Absorbs water, mineral salts and vitamins
- Faeces stored in rectum before being expelled
Diabetes
- Medical condition in which blood glucose levels remain persistently higher than normal
- Type 1 diabities
- Type 2 diabetes
- Gestational diabetes
| Type 1 | Type 2 |
|---|---|
| Cannot be prevented | Can be prevented via lifestlye modifications |
| Body does not create enough insulin | Body does not create enough insulin develops insulin resistance |
| Causes are unknown, but genetics may play a role | Causes include family history, aging, inactivity, obesity, and more |
| Requires insulin injections for life | Requires insulin as needed, injected or oral |
Similarities:
- Can cause serious health problems
- Requires healthy lifestyle and medical supervision
- Symptoms includes thirst, frequent urination, and blurry vision
Risk factors for Type 2 Diabetes:
- unhealthy diet
- overweiht
- physical inactivity
- old age
Blood Glucose Regulation
- When blood glucose concentration is high, the pancreas cells secrete insulin
Overview